Frailty is one of the most significant challenges in aged care today. It’s more than just physical weakness—it’s a complex condition that affects strength, mobility, cognition, and resilience. Residents living with frailty are more likely to fall, be hospitalised, and experience a lower quality of life. But frailty isn’t inevitable. With the right approach, it can be prevented, slowed, and in some cases, reversed.

The first step in reducing frailty is recognising it early. Screening tools like the Clinical Frailty Scale or FRAIL questionnaire can help care teams identify early warning signs. This allows for timely interventions that are tailored to the individual’s needs. Person-centred care is key—what works for one resident might not work for another.
Movement matters.
Regular, gentle exercise is one of the most effective tools we have. Even short daily walks, chair-based exercises, or physiotherapist-led balance and strength sessions can have a big impact. Keeping muscles strong helps prevent falls, supports independence, and improves mood. In facilities where allied health professionals are involved in daily care planning, residents benefit from more structured and safe activity programs.
Nutrition also plays a central role.
Many older adults in care are undernourished or not getting enough protein and essential nutrients. Dietitians can assess residents’ individual needs and work with kitchen staff to provide energy-dense, high-protein meals and snacks that are easy to chew and swallow. Supplements or fortified foods may be needed for some. A focus on hydration is also important, as dehydration can worsen confusion and fatigue—two common features of frailty.
Falls prevention must be front and centre.
Falls are often both a symptom and a cause of worsening frailty. A multifactorial approach includes regular medication reviews, vision and hearing checks, ensuring appropriate footwear, and modifying environments to reduce trip hazards. Exercise and strength training are proven to reduce fall risk. Nurses and care staff play a critical role in monitoring changes in balance, gait, and alertness—early signs that a resident might be at increased risk.
Nursing care is the backbone of frailty management in aged care.
Nurses are often the first to notice subtle changes—weight loss, increased fatigue, mood changes, or difficulty with mobility. Ongoing assessment, care coordination, and communication with families are essential. Nurses also manage complex care needs and work closely with GPs and allied health professionals to adjust care plans as residents’ needs evolve.
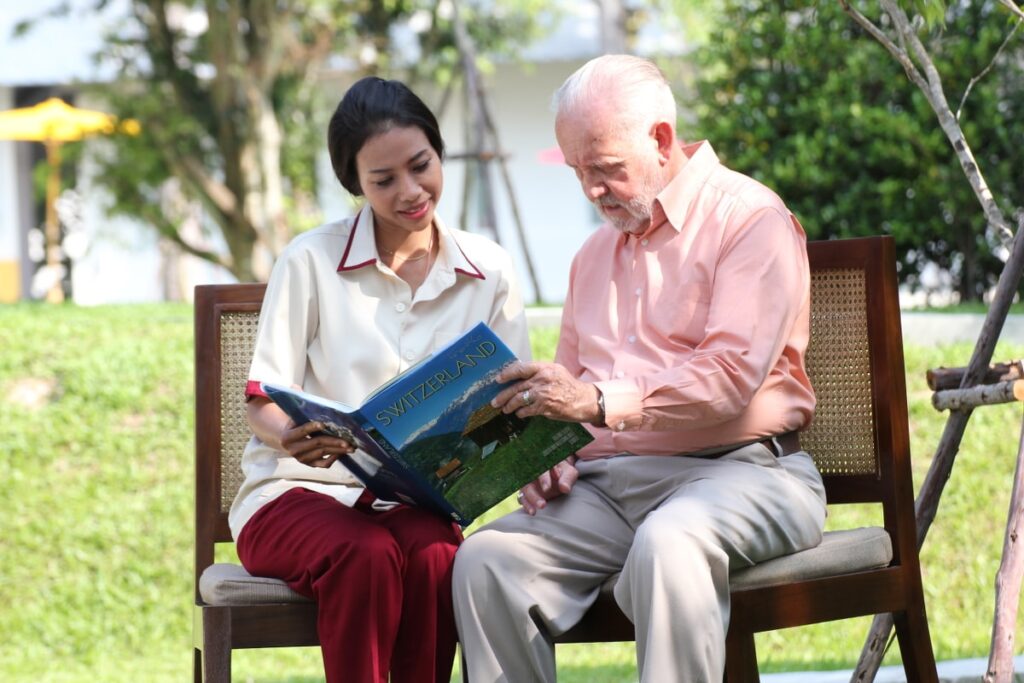
Reducing frailty also means addressing social and emotional well-being. Loneliness, grief, and depression can all contribute to physical decline. Encouraging regular social interaction, meaningful activities, and mental stimulation helps residents feel engaged and valued. Volunteers, chaplains, and lifestyle coordinators can make a big difference in this space.
Finally, collaboration is essential. Government programs and not-for-profit providers offer resources, staff training, and funding opportunities that can strengthen frailty care across the sector. When aged care homes foster partnerships with allied health providers, hospitals, and community services, residents receive more comprehensive and coordinated care.
Frailty doesn’t have to be a one-way path. With the right mix of movement, nutrition, falls prevention, proactive nursing, and social connection, aged care facilities can help residents age with strength, dignity, and purpose.
References:
- Clegg, A., Young, J., Iliffe, S., Rikkert, M. O., & Rockwood, K. (2013). Frailty in elderly people. The Lancet, 381(9868), 752–762. https://doi.org/10.1016/S0140-6736(12)62167-9
- Australian Commission on Safety and Quality in Health Care. (2021). Falls prevention in older people. Retrieved from https://www.safetyandquality.gov.au/
- Morley, J. E., Vellas, B., van Kan, G. A., et al. (2013). Frailty consensus: A call to action. Journal of the American Medical Directors Association, 14(6), 392–397. https://doi.org/10.1016/j.jamda.2013.03.022
- Healthdirect Australia. (2023). Frailty in older people. Retrieved from https://www.healthdirect.gov.au/frailty-in-older-people
- Dent, E., Martin, F. C., Bergman, H., Woo, J., Romero-Ortuno, R., & Walston, J. D. (2019). Management of frailty: Opportunities, challenges, and future directions. The Lancet, 394(10206), 1376–1386. https://doi.org/10.1016/S0140-6736(19)31785-4
- Visvanathan, R., & Wilson, A. M. (2017). Frailty in older people: A national health priority. MJA Insight. Retrieved from https://insightplus.mja.com.au/
- Hill, A. M., Etherton-Beer, C., & Haines, T. P. (2013). Tailored education for older patients to facilitate engagement in falls prevention strategies after hospital discharge—A pilot randomized controlled trial. PLoS ONE, 8(5), e63450. https://doi.org/10.1371/journal.pone.0063450
- Dietitians Australia. (2022). Nutrition and ageing: Fact sheet. Retrieved from https://dietitiansaustralia.org.au
- Australian Institute of Health and Welfare (AIHW). (2021). Older Australians at a glance. Retrieved from https://www.aihw.gov.au/reports/older-people/older-australia-at-a-glance